Amid the COVID-19 pandemic the B.C. Ministry of Finance has postponed a new tax on heated tobacco products that should have been implemented on April 1.
The government said it did not want to burden businesses with the new inventory requirements.
Public health researcher Dr. Kelley Lee of Simon Fraser University said while there may be some justification to delaying the tax, a more urgent priority should nevertheless be expansion of the government’s smoking cessation program.
“People currently smoking or vaping should be supported to quit now to give their lungs the best chance of fighting off this coronavirus if infected,” said Lee, who says these “sin” taxes not only serve to dissuade people from using products that compromise the lungs, but they can also be used as revenue for cessation programs.
The government did increase its tobacco tax by two cents a cigarette (to 29.5 cents) on January 1 and was intending to apply the same rate to heated tobacco units. It also created a new 20% provincial sales tax for vaping products on January 1.
Government also implemented stricter vaping advertisement and flavoured nicotine product guidelines to throttle the rising rate of vaping teenagers.
When asked if the government should ban cigarette sales by licensed retailers, Lee said such a measure could prove counterproductive; not only could it be cruel to those addicted to nicotine, the black market for cigarettes could expand.
Instead, Lee says a more obvious choice should be to expand the BC Smoking Cessation Program, which provides limited access to drugs, such as the “patch.”
“If the government wants to be helpful, increasing access to nicotine replacement therapy to help people quit is a far better way to go,” said Lee. This would also contribute towards flattening the curve by reducing the likelihood that smokers and vapers will get seriously ill and need to rely on our overstretched health system.”
But, when asked, the Ministry of Health did not respond if it is planning to expand the BC Smoking Cessation Program, which covers 100% of the cost of nicotine replacement therapy products (specifically nicotine gum, lozenges, patches and inhalers), or contributes to the cost of specific smoking cessation prescription drugs.
However, there are program limits. Each calendar year, eligible B.C. residents can only receive a single continuous course of therapy treatment for up to 12 weeks. And only low-income earners qualify for discounted prescription drugs. There is also a burdensome process of visiting a doctor for referral and registering for the program.
“So, for sure expand the cessation support to get that message out there — the link between COVID and smoking and vaping,” said Lee. “There’s kids out there vaping as well and they’re heavily addicted,” she added.
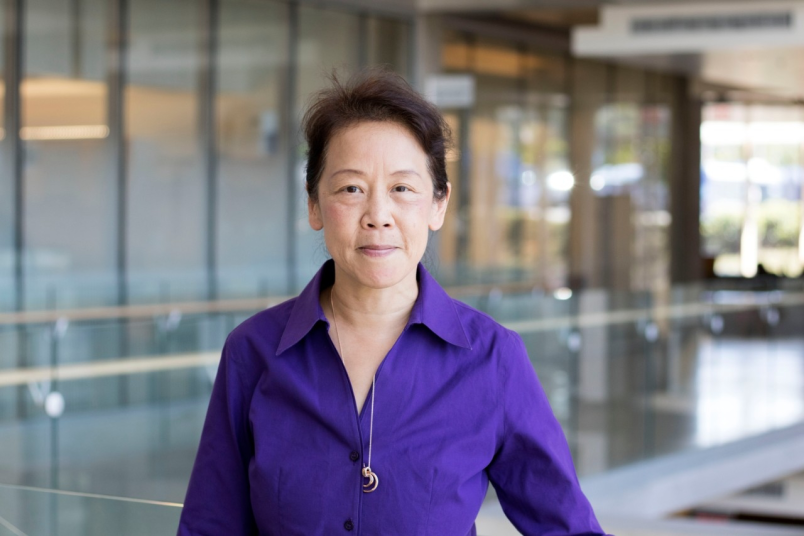
Lee researches and teaches about the role of globalization and health. She is a Fellow of the Faculty of Public Health, Royal College of Physicians and Fellow of the Canadian Academy of Health Sciences. Lee has specifically studied tobacco control for 25 years. She’s a leader of the Global Tobacco Control Programme at SFU and has conducted numerous studies with the World Health Organization.
The social scientist’s research focuses specifically on the impacts of globalization on communicable and non-communicable diseases (notably tobacco-related diseases) and the implications for strengthening global governance. As well, she is presently researching worldwide quarantine responses to COVID-19.
“My two worlds are coming together,” she said.
Lee is particularly concerned about the impact smokers and vapers could have on all healthcare systems during the pandemic.
“Anything that compromises your lung capacity is not wise at this time,” said Lee.
“By quitting smoking you’re probably going to increase your chances of being one of the people who gets a ventilator, for sure. I don’t think we’ve ever been in this situation where we have to make decisions so starkly,” as doctors have been doing in Italy and New York, said Lee.
“There’s going to be choices down the line if we don’t flatten the curve. It comes down to weighing who will fare better” from receiving help from equipment that is in short supply, said Lee.
Age, health history and other considerations come into play for who gets what care. If someone’s lungs are not at full capacity due to smoking or vaping, policy dictates they may be passed up in a worse case scenario, said Lee.
“There are concerns about the association between COVID-19 and tobacco use. There is emerging evidence that link those two things,” said Lee, suggesting smokers and vapers will have more severe illness from COVID-19. “They might have compromised lung capacity making it a more serious impact. This means they are less likely to have a mild case of illness.”
The B.C. Lung Association cites studies from China showing Chinese patients, who contracted COVID-19 and who have a history of smoking, were 14 times more likely to have disease progression and/or die. Overall, smokers are more likely to contract bacterial or viral infections, the association states.